Coronavirus (COVID-19) Pandemic: Personal Protective Equipment Preservation Best Practices
FEMA • April 15, 2020
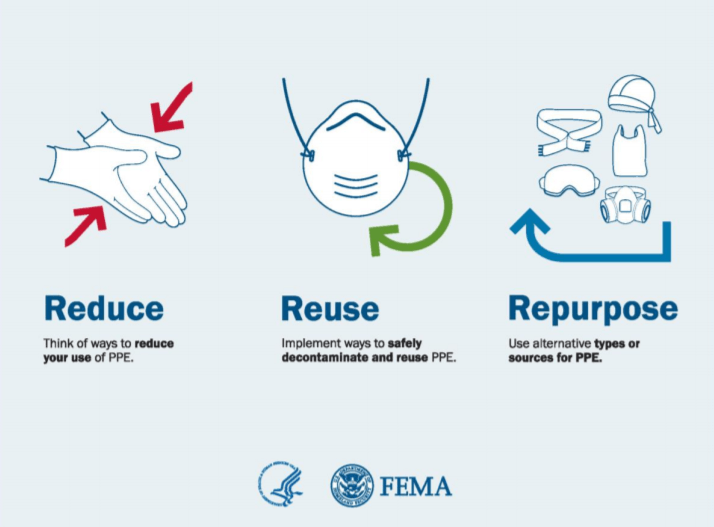
This guidance summarizes best practices for national implementation to sustain personal protective equipment (PPE) while ensuring the protection workers during the coronavirus (COVID-19) pandemic response.
Objective
The objective of the COVID-19 National Strategy for Addressing Personal Protective Equipment (PPE) Shortage is to
ensure protection against COVID-19 for healthcare workers, first responders, and patients by implementing three
pillars of practice: reduce – reuse – repurpose. Due to the COVID-19 pandemic response and associated PPE
shortages, implementation of contingency and crisis capacity plans may be necessary to ensure continued
availability of protective gear.
This fact sheet amplifies Centers for Disease Control and Prevention (CDC) strategies on conventional, contingency
and crisis capacity strategies for optimizing PPE. All U.S. healthcare facilities should begin using PPE contingency
strategies now and may need to consider crisis capacity strategies if experiencing PPE shortages.
What Do I Do and How Do I Do it?
- Reduce Usage Rate of PPE by Modifying Normal Operations and Procedures
- Limit the need for PPE by maximizing use of barrier controls whenever possible (e.g. masking patients,
- Plexiglas barriers, car windows and improved ventilation systems).
- Place IV towers and ventilators outside of patient rooms, as clinically appropriate, to enable appropriate monitoring and management without donning of PPE.
- Automate delivery of food and supplies.Use tele-consultation, internet-based interviews, or remote camera-based observation, as available.
- Limit visitor access and offer technology-enabled alternatives (e.g., video chat).
- Understand PPE requirements and burn-rates - cdc.gov/coronavirus/2019-ncov/hcp/ppe- strategy/burncalculator.html
- Consider extending use-times of undamaged, non-visibly soiled PPE beyond single patient contact and other standard practice durations.
- Note: OSHA has relaxed enforcement of annual fit-testing requirements for N-95 filtering facepiece respirators (FFRs) - osha.gov/news/newsreleases/national/03142020.
- Reuse PPE by Implementing Optimization, Decontamination, and Reuse Procedures
- Implement strategies to optimize supplies and equipment: cdc.gov/coronavirus/2019- ncov/hcp/ppestrategy/index.html
- Implement expanded facility-based PPE reuse policies and procedures.
- Track “check in” and “check out” of PPE designated for reuse. Each worker is provided specific PPE at the beginning of the shift. At the end of the shift, all PPE is labeled, collected, and stored forreuse (which may entail appropriate decontamination using devices with issued Food and Drug Administration (FDA) Emergency Use Authorization (EUA).
- Implement guidance for decontamination and reuse of FFRs:
- cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
- osha.gov/memos/2020-04-03/enforcement-guidance-respiratory-protection-and-n95- shortagedue-coronavirus
- For large-scale decontamination of N-95 FFRs consider using the following methods:
- Industrial or facility-based vaporized hydrogen peroxide sterilization systems: fda.gov/media/136529/download
- Industrial or facility-based moist heat disinfection systems (NOT autoclaves)
- Facility-based ultraviolet germicidal irradiation (UVGI) systems
- For low-volume or personal decontamination of N-95 FFRs consider using commercially available microwavable moist heat disinfection devices following manufacturer’s instructions (e.g. do not put metal parts in microwaves).
- Repurpose Alternative Types or Sources of PPE
- Use alternative NIOSH-approved respirators in lieu of N-95 FFR for activities for which respiratory protection is required. See fda.gov/media/135763/download. Examples include:
- powered, air-purifying respirators (PAPRs);
- reusable air-purifying respirators (elastomeric half and full facepiece respirators);
- other disposable air-purifying particulate FFRs.
- Contingency - Seek alternative supplies of PPE.
- Encourage community members to donate private stocks of unused/unopened surgical masks, gloves, gowns, and N-95 respirators to your facility.
- Seek PPE and other equipment from dentist offices, veterinarians, individuals, and other sources, including business that are not active.
- Use commercial sources of industrial Tyvek coveralls, face shields, goggles, shoe covers, etc.
- Crisis - Use N-95 FFRs beyond their expirations dates if certain conditions are met
- Crisis - Use FDA authorized imported, non-NIOSH-approved disposable FFRs.
Implementation
Organizations need to assemble a team to carefully review existing Health and Safety Plan (HASP) and Respiratory
Protection Plan (RPP) policies and procedures for opportunities to reduce, reuse, or repurpose and should develop
contingency and crisis operational plans. Such a team might include (where available) environmental health officers,
safety officers, industrial hygienists, logistics officers, infection prevention practitioners, operations chiefs, medical
officers, and work-force representatives.
To ensure uniform application of modified practices, processes and procedures, and, concurrently, the safety of
workers, all workers must be trained in the plans, with recommended elements of such training including:
- The rationale for changes, contingency and crisis standards during COVID-19 related PPEshortages
- New PPE guidance (FDA, CDC, DOJ) related to COVID-19
- Proper methods to conduct new or changed work practices (e.g., staffing, social distancing)
- Methods to install or utilize any barrier controls (e.g. patient masking, Plexiglas shields)
- Proper donning and doffing of PPE to minimize self-infection
- Proper hand hygiene

ETCOG announces that $3.1 million in grants from the Office of the Governor's (OOG) Public Safety Office have been awarded to East Texas jurisdictions and nonprofit organizations. These funds are aimed at enhancing public safety and supporting victims of crime. The program’s mission is to strengthen Texas communities by supporting initiatives that help victims recover and feel secure while also preventing crime through programs that: Prevent juvenile delinquency and support truancy prevention Provide services to victims of crime and address violence against women Support law enforcement and improve the criminal justice system Prevent child sex trafficking, bring justice to its perpetrators, and restore victims ETCOG's Public Safety Division assists jurisdictions in applying for these funds annually, and applications submitted for funding are ranked and scored by the ETCOG Criminal Justice Advisory Committee, which is comprised of local subject-matter experts from across the region. The following Victims of Crime Act, Justice Assistance, Violence Against Women Act, and Juvenile Assistance grants totaling $3,136,019.36 have been approved by the OOG for funding in East Texas: Victims of Crime Act Funds - $2,528,962.18 The Crime Victims Assistance Grant Program (VOCA) devotes resources to providing direct services to victims of crime to help them recover and navigate the justice system.